The NHS Long Term Plan (LTP) sets the ambition that, from 2028, an extra 55,000 people each year will survive for five years or more following their cancer diagnosis, and three in four cancers (75%) will be diagnosed at an early stage.
Faster and more efficient cancer pathways will not achieve these ambitions on their own. However, they have a crucial contribution to make. By getting patients from referral to diagnosis more quickly we can increase the chance of an early stage diagnosis. Pathway Improvements can also indirectly support earlier diagnoses by widening access, providing a platform for piloting and adoption of innovations such as self-referral routes, and reducing barriers between primary and secondary care.
It is clear that the number of people investigated for suspected cancer will continue to rise, both as a result of demographic change and as a result of actions taken to target the Early Diagnosis ambition. Efficient, patient-centred, pathways that allow clinicians to focus on the rapid investigation of the highest priority patients, whilst allowing fast and effective rule out and management of those without cancer will become ever more important.
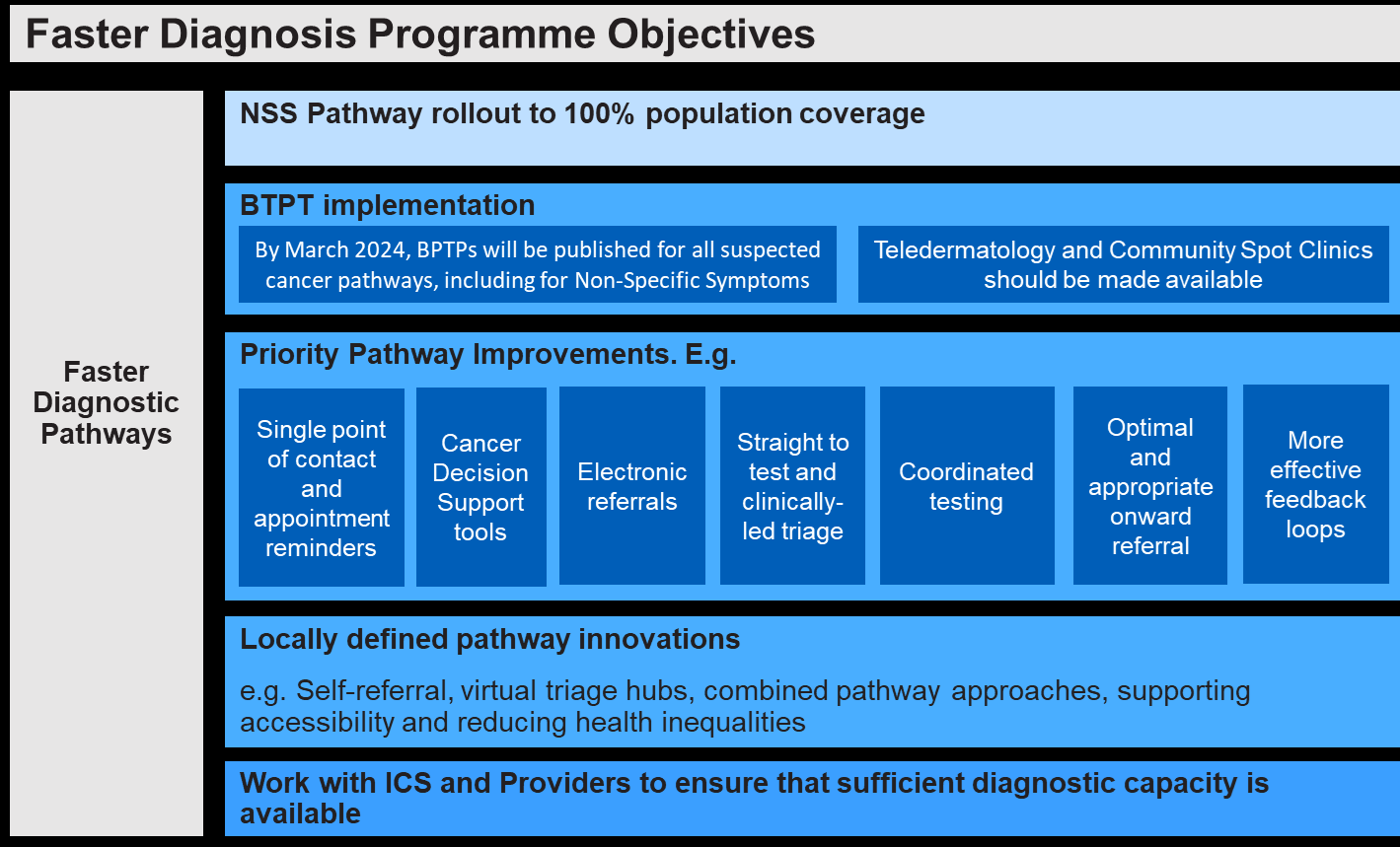
Cancer Alliances have been tasked with achieving the following five key objectives:
- Complete the rollout of Non-Specific Symptom pathways to achieve 100% population coverage by March 2024.
- Implement the sequencing of pathways and achieve the maximum timeframes of all published FDS Best Practice Timed Pathways.
- Implement a set of core improvements across all cancer pathways, regardless of tumour type so that every cancer patient gets the right tests at the right time in as few visits as possible, including:
- Patients will be navigated through their pathway via a single point of contact with SMS/email appointment reminders.
- Cancer Decision Support (CDS) tools are available to access for all GPs. • All urgent suspected cancer referrals are made electronically.
- Straight to test and clinically led triage models in place to streamline the beginning of the pathway.
- Coordinated testing to minimise the number of locations and appointments a patient must attend.
- Processes to ensure appropriate onward referral/discharge, whether or not a patient is diagnosed with cancer.
Guidance to GPs and more effective feedback loops to support effective and accurate referrals, with all referrals accompanied by effective minimum datasets.
Faster Diagnosis Activities to date
In 2021, the 28 Day Faster Diagnosis Standard (FDS) was introduced to replace the current Two Week Wait (2WW) standard as recommended by the Independent Cancer Taskforce. The FDS sets a maximum 28-day wait for communication of a cancer diagnosis or ruling out of cancer for patients referred urgently for investigation of cancer (including those with breast symptoms) and from NHS cancer screening. Enabling systems to meet this standard through an aligned strategic approach to Faster Diagnosis, is a priority for the NHS cancer programme and will support patients care and service capacity.
Since 2018, Best Practice Timed Pathways (BPTPs) have been developed by expert clinical “task and finish” groups. These groups have outlined the best evidenced structure and timing of various tumour-specific pathways to meet the Faster Diagnosis Standard. These BPTPs identify specific clinical events and tests for patients referred with defined NG12 symptoms. Delivery of the timed pathways will support the highest quality care for patients and reduce variation in patients accessing diagnostics, improving treatment options and outcomes.
Since 2019, Cancer Alliances have been developing new pathways for patients with non-specific symptoms (NSS) that can indicate cancer. Non-Specific Symptoms pathways are intended to cover the cohort of patients who do not fit clearly into a single ‘urgent cancer’ referral pathway, as defined by NG12, but who are, nonetheless, at risk of being diagnosed with cancer. Symptoms considered ‘non-specific’ include unexplained weight loss, fatigue, abdominal pain or nausea; and/or a GP ‘gut feeling’ about cancer. Historically, this cohort of patients often:
- saw their GP multiple times before referral
- presented more often in an emergency setting
- presented with late-stage cancer and
- were referred on multiple urgent pathways with resulting inefficiencies in healthcare provision.
